Neuroplasticity in Action: How You Actually “Rewire” Your Brain
The Brain Is Not Hard-Wired: Debunking the Old Myth
For decades, the standard medical teaching was that the adult brain was a "finished product." We were told that by the time you hit your mid-twenties, your neural hardware was locked in. If you struggled with chronic anxiety, depression, or the long-term echoes of trauma, the outlook was often focused on "coping" rather than "evolving."
I am so happy to tell you that this old narrative is officially outdated.
Neuroplasticity is the brain’s lifelong ability to physically reorganize itself. It means your brain is a dynamic, living organ that responds to your environment, your thoughts, and your habits. Whether you are 25 or 75, your brain is capable of forming new connections and even growing new cells.
To visualize this, I always suggest the hiking trail analogy. Think of your brain as a lush, dense forest. Your habitual thoughts—like that "inner critic" or an automatic stress response or anxiety loop—are like well-worn, paved footpaths. Change doesn't happen by "erasing" the old path; it happens by intentionally blazing a new trail through the undergrowth. At first, it’s exhausting and the path is thin. But with every step you take, the new trail becomes wider and the old, unused path slowly grows over. Neutral pathways strengthen in a similar manner.
The Anatomy of Change: What’s Happening Under the Hood?
When we talk about "rewiring," we aren't just being poetic. Change happens at several levels:
Synaptic Plasticity: This is the most basic level. When two neurons communicate frequently, the "handshake" between them becomes stronger. As we say: "Neurons that fire together, wire together." The reverse is also true—connections that are not used gradually weaken.
Structural Changes: Research shows that consistent practices can increase the volume of the Hippocampus (memory/emotion) and the Prefrontal Cortex (logic/impulse control). This could be through therapy, learning, and mindfulness practices.
Neurogenesis: The brain can birth new neurons, essentially "building new hardware" to support your recovery. This process is strongly influenced by lifestyle factors such as exercise, sleep, stress reduction, and novelty.
Synaptic plasticity refers to how neurons communicate
Neuroplasticity is the broad concept of the brain's ability to change, while synaptic plasticity is a specific, fundamental mechanism within neuroplasticity
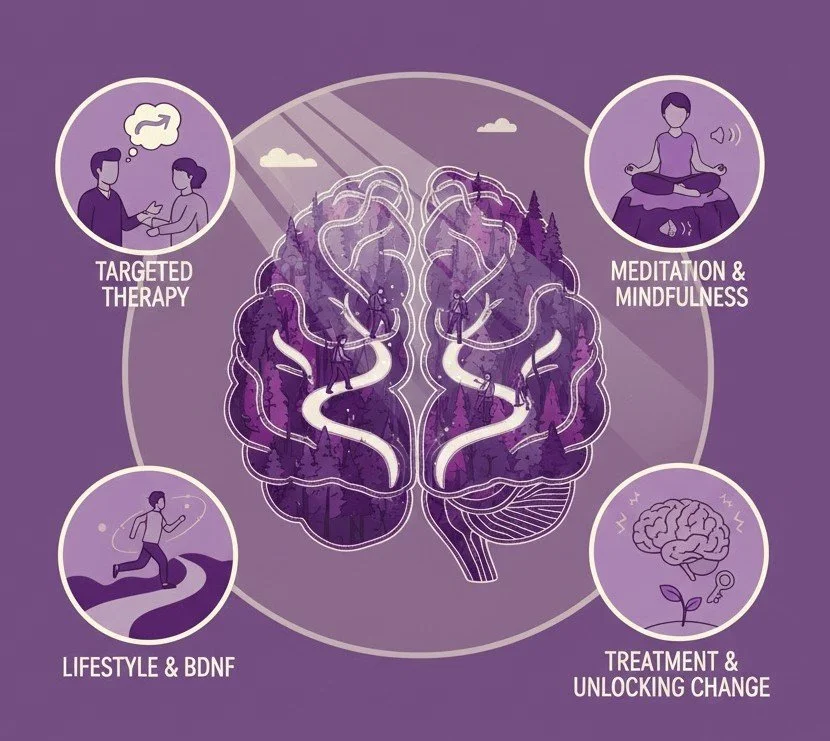
Pillar 1: Targeted Therapy & The “Manual” Rewire
In my work here at Kleya Psychiatry, I view therapy as a structured way to guide this biological rewiring. While I do not specifically offer individual 1:1 psychotherapy WITHOUT medication management, I do integrate it into my practice, weaving it in with medication and psychiatric visits and encourage all of my clients to also see an individual therapist to help reinforce their recovery efforts.
Breaking the Loop: Many emotional struggles persist because the brain is stuck in a loop—automatic negative thoughts, trauma responses, or rigid beliefs that once served a purpose but no longer do. Modalities like talk therapy and Cognitive Behavioral Therapy (CBT) help us identify these "maladaptive" pathways—the "bugs" in your mental code.
Cognitive Reframing: By consciously choosing a more accurate thought, you are manually steering your neural firing away from the old trail and onto the new one. Each time this new thought is practiced, the old neural loop weakens and the new one strengthens.
Psychedelic Integration: In psychedelic integration work, this process can accelerate. Psychedelic experiences may create a temporary window of heightened plasticity, during which the brain is more flexible and receptive to change. This allows us to reshape the landscape of your mind much faster. Integration ensures those changes stick.
Pillar 2: Meditation (The Architect of Calm)
Mindfulness is often misunderstood as "clearing the mind." In reality, it is resistance training for your brain. It strengthens the "CEO" (Prefrontal Cortex) and shrinks the "Alarm" (Amygdala). Mindfulness is not passive—it is active brain training.
Consistent mindfulness practices have been shown to reduce activity and even decrease gray matter density in the amygdala, the brain’s alarm system responsible for fight‑or‑flight reactions. This doesn’t eliminate fear; it reduces over‑reactivity.
At the same time, meditation strengthens the prefrontal cortex, improving attention, impulse control, and emotional regulation. This is why mindfulness often leads to more thoughtful responses rather than automatic reactions.
Meditation also impacts the Default Mode Network (DMN)—the brain network associated with rumination, self‑criticism, and mind‑wandering. By quieting the DMN, mindfulness helps create mental space and reduces the constant internal noise that fuels anxiety and depression.
Because I know sitting still can be a challenge—especially when your brain feels "noisy"—I like to offer my patients a variety of ways to practice.
My Favorite Meditation Techniques:
The 2-Minute Breath Anchor: Sit comfortably. Focus on the air entering your nostrils or the rise of your belly. When your mind wanders (and it will!), simply notice it, label it "thinking," and gently return to the breath. Or go beyond “thinking”- label it: “planning,” or “worrying,” then return to breath. This "return" is the actual muscle-building moment for your brain. Mindfulness is purposeful, present‑moment attention with an attitude of non‑judgment. In practice, it is a form of attention training: noticing where the mind goes and gently returning it to an anchor (often the breath). This repeated cycle strengthens attentional control and emotion regulation.
Box Breathing: Inhale for 4 seconds, hold for 4, exhale for 4, and hold for 4. This rhythm sends a physical signal to your nervous system that you are safe, manually "switching off" the fight-or-flight response.
Walking Meditation: You don't have to be still. While walking, focus entirely on the sensation of your feet hitting the ground. Notice the shift in weight from heel to toe. This is a great way to practice if you have a lot of "fidgety" energy.
Why this works (in plain terms)
Trains attention regulation and reduces mind‑wandering
Lowers perceived stress even in brief programs
Supports emotion regulation via fronto‑limbic networks
Mindfulness doesn’t require long sessions. Two minutes, repeated, builds the habit and delivers measurable benefit. Consistency beats duration.
Pillar 3: Lifestyle & “Brain Fertilizer” (BDNF)
If therapy is the "roadmap," then Brain-Derived Neurotrophic Factor (BDNF) is the "Miracle-Gro." Therapy and insight need the right biological environment to take root. A key player is Brain‑Derived Neurotrophic Factor (BDNF), a protein that acts like Miracle‑Gro for neurons. BDNF supports synaptic growth, learning, and resilience.
New Insights into BDNF Research
Movement is Medicine: New research suggests that "Vigorous Intermittent Lifestyle Physical Activity" (short, intense bursts of movement) can spike BDNF almost as effectively as a long gym session.
The Sleep-Cleaning Crew: During deep sleep, your brain "prunes" unnecessary connections. Without sleep, BDNF cannot "pave" the new trails you worked on during the day.
The Gut-Brain Axis: Chronic inflammation in the gut can "stunt" BDNF production. A brain-healthy diet isn't about weight; it's about keeping the brain "plastic" and flexible. The gut‑brain axis plays a major role in neurotransmitter production and inflammation, both of which influence mood, focus, and emotional stability.
Ketamine & Rapid Plasticity: One reason Ketamine has been such a breakthrough is its ability to cause a rapid spike in BDNF, essentially "unlocking" a brain that has been stuck in a rut for years.
When Plasticity Gets Stunted
Mental illness isn't a lack of willpower. Chronic stress releases cortisol, which can "wither" the prefrontal cortex while strengthening the "fear" circuits. Your brain gets really good at being anxious. This is why a holistic psychiatry approach is vital—we have to biologically "unlock" the brain so it becomes flexible enough to heal.
Neuroplasticity is impaired in mental illness through chronic stress, which reduces BDNF and synaptic density, and via neuroinflammation and microglial dysregulation that disrupt synaptic pruning and plasticity. Early-life adversity and trauma can prematurely close sensitive periods, limiting later adaptive plasticity. Genetic and epigenetic factors (e.g. BDNF polymorphisms, miRNA dysregulation) further constrain plasticity, while maladaptive plasticity entrenches dysfunctional circuits in depression, schizophrenia, and addiction. These deficits manifest as reduced synaptic plasticity, impaired learning, and rigid, maladaptive behaviors. Read more about this below…
-
Brain-derived neurotrophic factor (BDNF) dysregulation: Chronic stress and depression reduce BDNF, a key mediator of synaptic plasticity, leading to decreased synaptic density and impaired neural connectivity
Synaptic dysfunction: Mental health conditions such as depression and schizophrenia exhibit reduced synaptic density and impaired synaptic signaling, particularly in the prefrontal cortex and hippocampus
Neuroinflammation: Chronic inflammation and microglial activation disrupt synaptic pruning and plasticity, contributing to cognitive and emotional impairments
Epigenetic modifications: Early-life adversity and chronic stress induce epigenetic changes that alter gene expression related to neuroplasticity, including BDNF and other synaptic proteins
-
Hippocampal atrophy: Chronic stress and depression are linked to reduced hippocampal volume, a region critical for memory and emotional regulation
Prefrontal cortex abnormalities: Reduced gray matter volume and impaired connectivity in the prefrontal cortex are observed in depression, schizophrenia, and bipolar disorder
White matter alterations: Disruptions in white matter integrity, particularly in fronto-limbic circuits, are associated with impaired emotional regulation and cognitive function
-
Hypoactivation of prefrontal cortex: Reduced activity in the prefrontal cortex, a region involved in executive function and emotional regulation, is observed in depression and schizophrenia
Hyperactivation of limbic regions: Increased activity in the amygdala and other limbic structures is associated with heightened emotional reactivity and stress responses .
Impaired functional connectivity: Disrupted connectivity between prefrontal and limbic regions underlies rigid, maladaptive cognitive and emotional processing patterns
-
Chronic stress: Persistent stress exposure impairs neuroplasticity by reducing BDNF, promoting neuroinflammation, and altering synaptic structure and function
Early-life adversity: Childhood trauma and neglect disrupt normal neurodevelopment, leading to long-lasting impairments in neuroplasticity and increased vulnerability to mental illness
Substance abuse: Chronic drug use induces maladaptive plasticity in reward circuits, contributing to addiction and comorbid mental health disorders
How We Open the Windows of Change: A Review of Effective Treatment Options
Understanding that your brain can be "un-stuck" changes how we look at treatment. My goal at Kleya Psychiatry is to help you find the right tool—or combination of tools—to help those new neural trails take root. Here is how our modern treatments actually work with your brain’s biology:
Traditional Medications (like SSRIs or SNRIs): Think of these as a slow-release "brain tonic." They work by gradually increasing your BDNF levels and helping your neurons remodel themselves over time. While they often take a few weeks to kick in, they provide a steady foundation for long-term rewiring.
Rapid-Acting Options (like Ketamine): For those who need a more immediate shift, treatments like Ketamine act like a "jumpstart" for neuroplasticity. They can rapidly increase the number of connections between your neurons, often providing a lift in mood within hours and opening a vital "window" where therapy can be even more effective. While I do not offer IV, IM, or intranasal Ketamine- a referral to a reputable clinic can be provided. Additionally, sublingual Ketamine lozenges may be an option here at Kleya.
The Power of Therapy: While medication can help "fertilize" the soil, Cognitive Behavioral Therapy (CBT) is the actual gardening. By intentionally practicing new ways of thinking, you are physically guiding your brain to strengthen healthy circuits and let the old, painful ones fade away.
Non-Invasive Brain Stimulation: For some, we might discuss techniques like TMS (Transcranial Magnetic Stimulation). These tools use gentle magnetic pulses to "wake up" specific areas of the brain that have become underactive, helping to restore the natural flow of communication between your neural networks.
Conclusion: You Are the Architect
Your current mental state is not your permanent destination. Rewiring a brain takes time, repetition, and a lot of self-compassion. At Kleya Psychiatry, we use medication to clear the fog, therapy to map the route, and lifestyle to fertilize the ground.
Are you ready to begin your journey of neurological transformation?
I am here to help you navigate this journey, one new trail at a time. Contact Kleya Psychiatry today and let’s start your manual rewire together.