PTSD: Why It Can Feel Like Anxiety, Depression, or Something Else Entirely
At Kleya Psychiatry, I often hear patients say, “I’ve been treated for anxiety or depression for years, but something still doesn’t feel right.” For many people, that missing piece is trauma.
Post‑Traumatic Stress Disorder (PTSD) is commonly misunderstood. It doesn’t always look like what we see in movies, and it often overlaps with other mental health conditions. Because of this, PTSD can go unrecognized for years, leaving people confused, frustrated, or blaming themselves for symptoms that don’t seem to fully improve. This post is meant to help you understand PTSD more clearly—both emotionally and biologically—and why it can look like so many other conditions.
What Is PTSD, Really?
PTSD is not a sign of weakness or an inability to “move on.” It is the nervous system’s response to experiences that felt overwhelming, frightening, or unsafe. Trauma can be a single event, such as an accident or assault, or it can be ongoing, like childhood neglect, emotional abuse, medical trauma, or chronic stress.
When the brain detects danger, it shifts into survival mode. In PTSD, that survival response doesn’t fully turn off. Even long after the threat has passed, your body and brain may continue reacting as if danger is still present—despite knowing logically that you’re safe.
Common PTSD Symptoms (In Everyday Language)
PTSD affects emotions, thoughts, physical sensations, and behavior. Common experiences include:
Re-experiencing: Your brain hits "replay" on the worst moments at the worst times (nightmares or intrusive memories).Avoidance: staying away from certain people, places, conversations, thoughts, or feelings
Avoidance: You start ghosting certain people, places, or even your own thoughts because they feel "spicy" or dangerous.
The "Mehs" & "Oof": Deep shame, emotional numbness, or feeling like the world is fundamentally a dumpster fire.
Hyperarousal: Feeling "on" 24/7. You’re jumpy, irritable, and sleep is a distant memory.
Not everyone experiences all of these symptoms, and they can change over time.
A Note on Dissociation: If you ever feel "foggy," "numb," or like you’re watching your life through a foggy window—that’s dissociation. It’s your brain’s way of pulling the fire alarm to save you from feeling too much. It’s not "weird"; it’s a protective mechanism.
What Trauma Does to the Brain and Nervous System
Trauma doesn’t just affect memories—it changes how different parts of the brain communicate. These changes are protective at first, designed to keep you alive, but they can become exhausting and disruptive when they persist.
Trauma doesn’t just affect memories—it changes how different parts of the brain communicate. These changes are protective at first, designed to keep you alive, but they can become exhausting and disruptive when they persist.
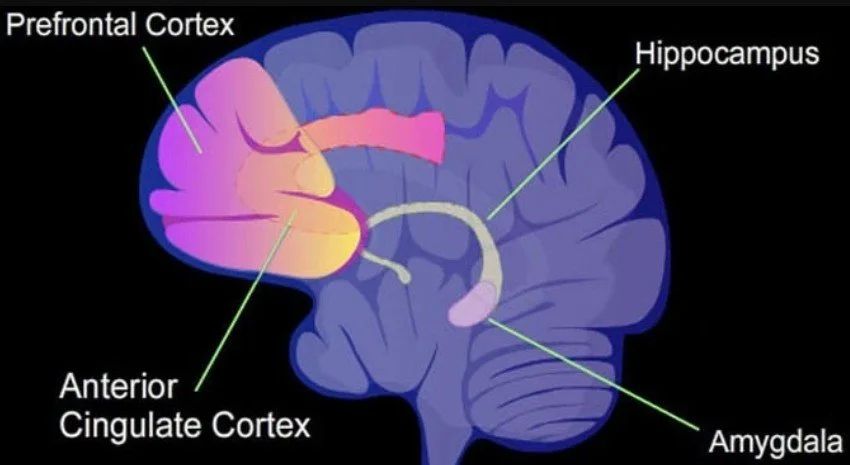
Several key brain regions are involved
-
Becomes overactive, making you more sensitive to potential threats. This contributes to hypervigilance, panic, exaggerated startle responses, and intense emotional reactions.
In PTSD, this guy is caffeinated and paranoid. It sees a minor inconvenience and screams, "ABANDON SHIP!"
-
Has a harder time calming the alarm system. This can make it difficult to regulate emotions, think clearly under stress, or reassure yourself that you’re safe.
This part usually says, "Chill, it’s just a car backfiring." In PTSD, the Adult is currently locked in a closet, making it hard to regulate emotions.
-
Helps organize memories and distinguish past from present. In PTSD, trauma memories may feel fragmented or intrude into the present as if they’re happening now.
A memory from ten years ago feels like it’s happening right now.
-
Involved in processing emotional pain and self‑evaluation. Changes here can increase emotional distress, self‑blame, and difficulty shifting out of intense feelings.
-
Becomes more sensitive and hyper-aware of your racing heart or that "pit" in your stomach, making anxiety feel like a physical emergency
The Biology Neurotransmitter systems implicated in PTSD
We can’t talk about PTSD without mentioning the HPA Axis—your body’s internal thermostat for stress. In PTSD, the thermostat is broken. PTSD also involves dysregulation of several neurotransmitter systems
The hypothalamic-pituitary-adrenal (HPA) axis, a major stress-response system, is frequently dysregulated in PTSD
Cortisol: Often weirdly low or dysregulated, meaning you don't "bounce back" from stress correctly.
Norepinephrine: This is at 11/10, keeping you shaky and alert.
GABA: The brain's "natural Valium" is often low, making it impossible to relax.
Serotonin (5-HT): Altered serotonin function is linked to mood dysregulation, anxiety, and impulsivity in PTSD .
Gamma-aminobutyric acid (GABA): Reduced GABAergic inhibition may underlie hyperarousal and anxiety symptoms .
Glutamate: Abnormal glutamatergic transmission is implicated in fear learning, extinction, and memory consolidation disturbances .
Together, these changes help explain why PTSD affects both the mind and the body—and why symptoms often feel automatic or out of your control.
Why PTSD Often Looks Like Other Mental Health Conditions
Because trauma touches everything—sleep, mood, attention—it’s the ultimate master of ceremonies for other diagnoses. This doesn’t mean your other diagnoses are "wrong," but they might be symptoms of a larger root cause.
How PTSD Overlaps With Other Conditions
PTSD shares neurobiological features with several other psychiatric conditions, contributing to symptom overlap and diagnostic challenges:
PTSD and Anxiety Disorders: Constant worry and panic
Both can involve excessive worry, panic, avoidance, and physical tension
In PTSD, these symptoms are often linked to trauma reminders and a persistent sense of threat
Shared hyperactivation of the amygdala and hypoactivation of the PFC contribute to excessive fear, hypervigilance, and avoidance behaviors
PTSD and Depression: Fatigue, numbness and withdrawal
Low mood, withdrawal, fatigue, and sleep changes occur in both
PTSD often includes emotional numbness, deep shame, and feeling disconnected from yourself or others
Overlapping features include hippocampal volume reduction, altered HPA axis function, and dysregulated serotonin and norepinephrine systems
PTSD and ADHD: Fidgeting and “zoning out”
Difficulty concentrating, restlessness, and mental fog can be trauma responses
A key difference is timing—ADHD symptoms usually begin in childhood, while trauma‑related attention problems often start after a distressing experience
Trauma-related attention difficulties may reflect altered prefrontal and parietal activity, distinct from developmental ADHD
Trauma makes it hard for the brain to focus because it's too busy scanning for danger.
PTSD and Bipolar Disorder: Irritability and sleep issues
Irritability and sleep disruption can overlap
In PTSD, mood shifts are typically triggered by reminders of danger or emotional overwhelm rather than distinct mood cycles
Bipolar disorder: Irritability and sleep disturbances in PTSD may involve overlapping neurobiological mechanisms, though the underlying pathophysiology differs
PTSD is complicated and is characterized by distinct neurobiological alterations involving fear and stress circuits, neurotransmitter systems, and neuroendocrine pathways.
These changes explain the symptom overlap with other psychiatric conditions and underscore the importance of trauma-informed, neurobiologically informed treatments for recovery
Why This Matters for Healing
Understanding the science helps shift the internal dialogue from "What is wrong with me?" to "What happened to my nervous system?"
Healing isn’t about deleting your memories like an old hard drive. It’s about teaching your brain and body that the war is overClinical implications and treatment considerations
How we do that:
Trauma-Informed Care: No one likes to be re-traumatized in therapy. We go at your pace.
Evidence-Based Therapy: Tools like EMDR or Cognitive Processing Therapy help the "Librarian" (Hippocampus) finally file those memories away correctly.
Smart Meds: Using medications to balance that overactive Norepinephrine or boost Serotonin so you can actually get a night's sleep.
Why Getting the Right Diagnosis Matters
When trauma is at the root, treatment needs to be trauma‑informed. Medication can be helpful for some symptoms, but psychotherapy that focuses on safety, nervous system regulation, and trauma processing is often essential. When trauma is overlooked, people may feel discouraged or blame themselves for not improving.
You’re Not Broken. You’re Responding.
If this post feels like I’m reading your diary, know that you aren’t "imagining things." Your symptoms make perfect sense given what you’ve survived.
Ready to stop living in survival mode?
At Kleya Psychiatry, I approach these conversations with curiosity and a healthy dose of respect for your story. You deserve a diagnosis that actually fits, and a treatment plan that helps you feel like you again.
You deserve care that understands the full picture. If you’d like to learn more or explore trauma‑informed treatment options, I’m here to help.