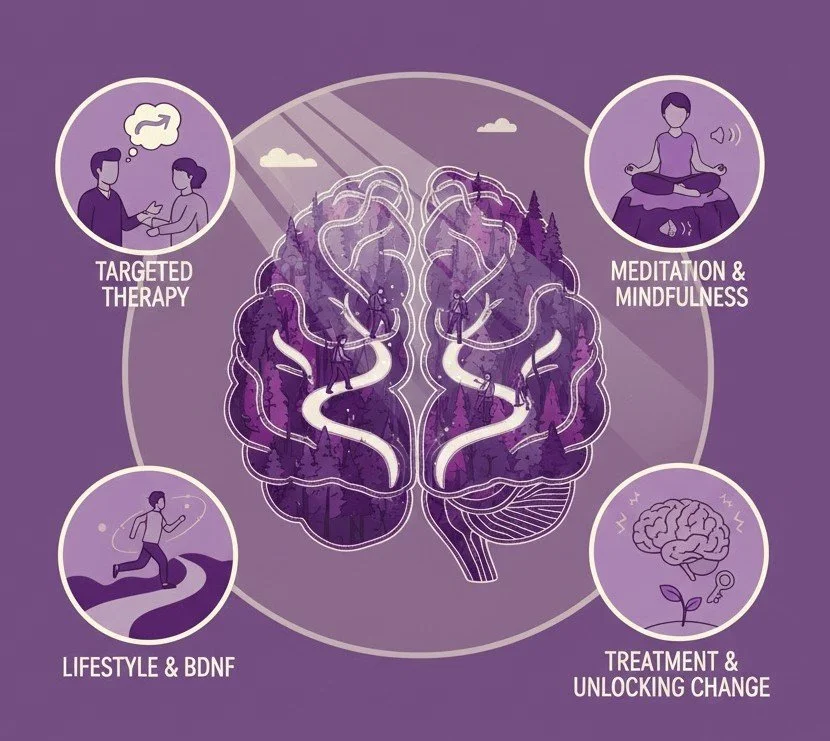
Neuroplasticity in Action: How You Actually “Rewire” Your Brain
For decades, neuroscience taught us that once adulthood was reached, the brain was essentially set in stone. If you developed anxiety, depression, or unhelpful coping patterns, the assumption was that you simply had to “manage” them.
We now know that belief is outdated.
Neuroplasticity is the brain’s lifelong ability to change—structurally and functionally—by forming new neural connections. Your brain is constantly adapting to what you think, feel, practice, and repeat.
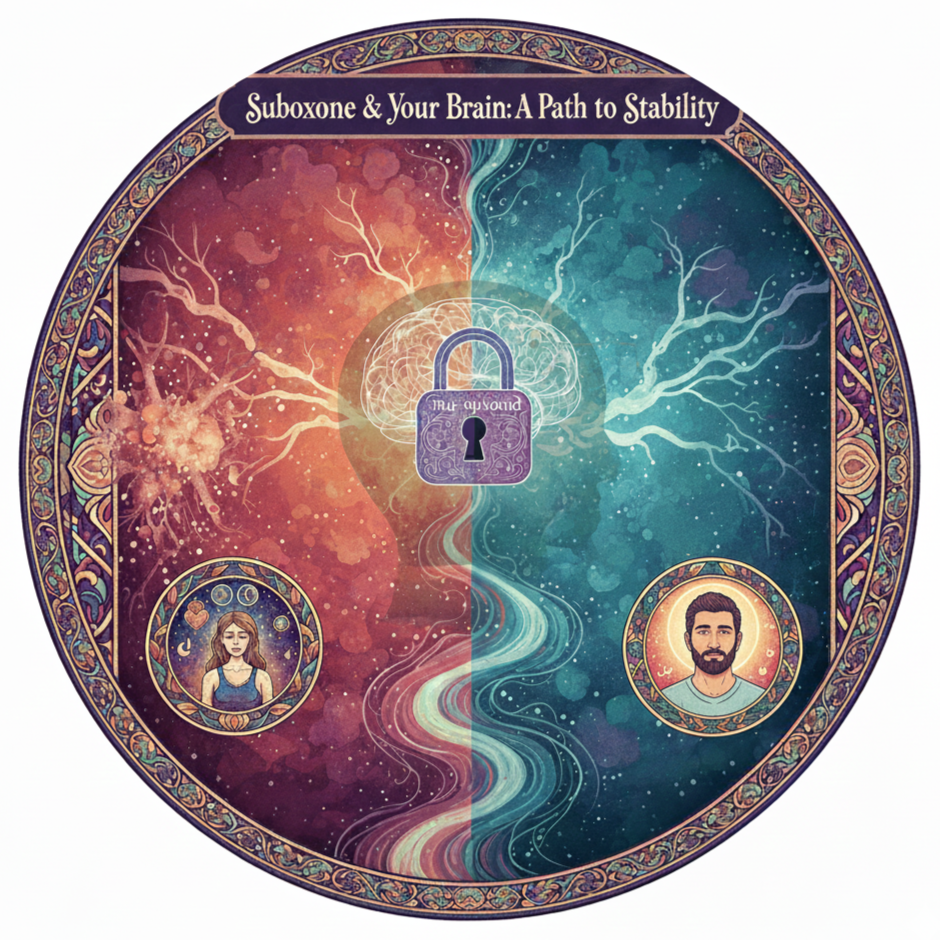
Beyond the Cycle: How Suboxone Supports Recovery from Opioid Use Disorder
If you or someone you love is navigating the complexities of opioid use—whether it began with a prescription for chronic pain or involves substances like heroin or fentanyl—you know how heavy the burden can feel. The constant cycle of withdrawal and cravings can make a "normal" life feel out of reach. At my practice, I view Opioid Use Disorder (OUD) not as a failure of willpower, but as a manageable chronic medical condition. Suboxone is one of the most effective tools I use to help my patients regain their footing and focus on the lives they want to lead.
Why Sleep Is One of the Most Powerful Tools for Mental Health
Sleep is not a luxury or an afterthought—it is foundational to mental health. Addressing insomnia directly is one of the most evidence‑based ways to support long‑term psychiatric recovery.
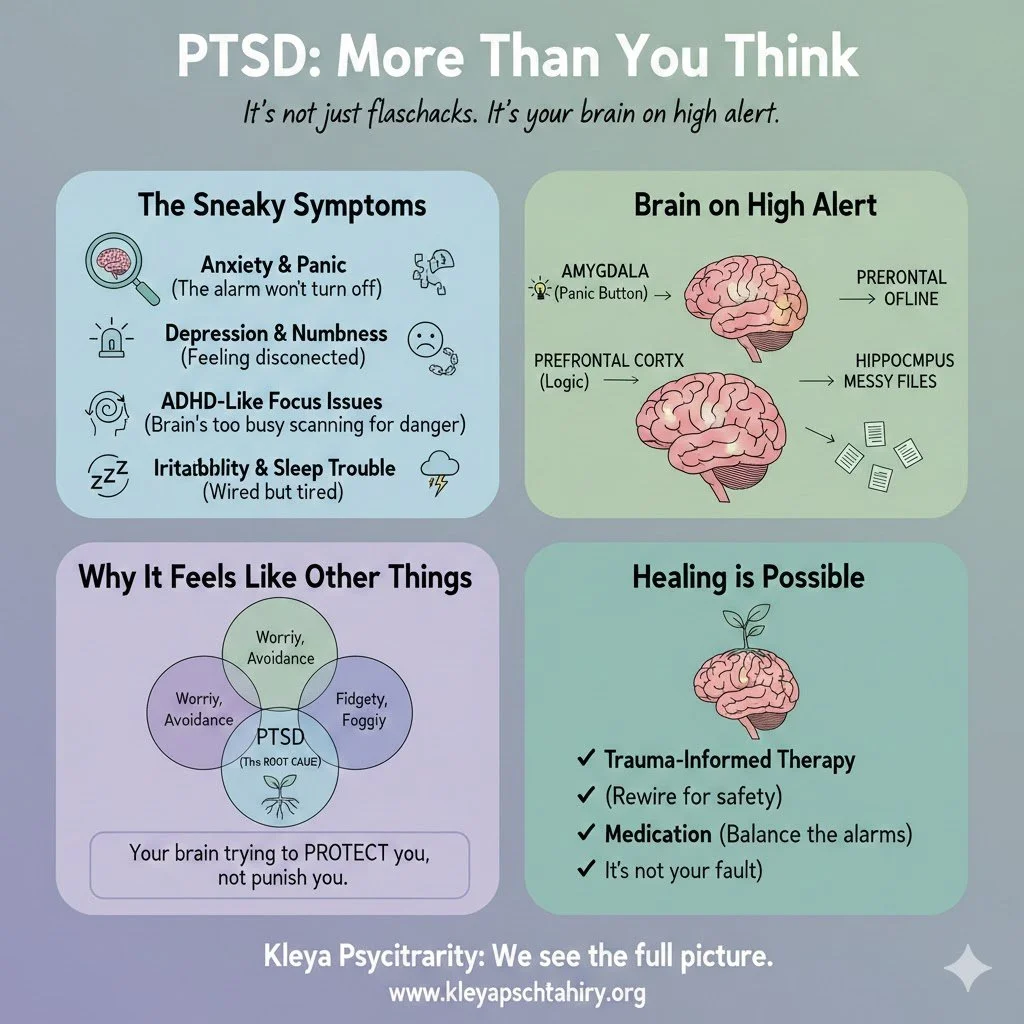
A Psych NP’s Guide to Why You Think You Have ADHD
Getting the diagnosis right is absolutely crucial. Treating an anxiety disorder with ADHD medication, or trying to manage ADHD without treating underlying sleep apnea, is like using a butter knife to fix a broken engine—it’s just going to be a messy, frustrating disaster.
So, You Think You Have ADHD?
So, You Think You Have ADHD?
Let's Talk About What That Really Means
Ever feel like your brain is running on three different channels at once, while simultaneously misplacing your keys for the tenth time this week? You're not alone.
If you've tumbled down the rabbit hole of self-diagnosis, wondering, "Is this just 'adulting,' or is it ADHD?", you are joining a massive club. Many bright, capable adults find themselves battling a persistent, invisible wall when it comes to focus, organization, or simply slowing down. So, let's take a pit stop at the mental health highway and figure out what an official ADHD diagnosis truly signifies.
Breaking Down the ADHD Blueprint: ADHD stands for Attention-Deficit/Hyperactivity Disorder. It’s not a character flaw or a trendy excuse…
Beyond the Pills: Why My Role as a Psychiatric Nurse Practitioner is Essential to My Vision for Your Recovery
What are PMHNPs? What is the benefit of having a dual certified psychiatric and medical nurse practitioner?
I am proud to have dual-certification as both a Psychiatric and Family Nurse Practitioner (FNP/PMHNP), as this combination truly embodies the gold standard of holistic care. This means I am uniquely equipped to identify symptoms stemming from physical health issues that may be mistaken for mental illness, and vice-versa. Having this integrated expertise ensures that your care is coordinated, comprehensive, and ultimately safer, eliminating the need to constantly relay information between separate mental health and primary care providers.
A Game-Changer in Addiction Treatment? Exploring GLP-1 Agonists for Alcohol Use Disorder
Observational data consistently show lower alcohol consumption and fewer alcohol-related events with GLP-1 RAs. Retrospective human studies—where researchers look back at the medical records of patients—have provided encouraging insights. For individuals being treated with GLP-1 RAs for obesity or diabetes, clinicians began to notice a pattern: many reported a spontaneous reduction in their desire for alcohol. Some reported that alcohol simply "tasted different" or that the rewarding buzz they once sought was diminished.